Osteoporotic vertebral fracture: Our Experience and update
DOI:
https://doi.org/10.3126/egn.v5i01.68444Keywords:
Osteoporotic Vertebral Fracture, Backpain, Conservative Management, SurgeryAbstract
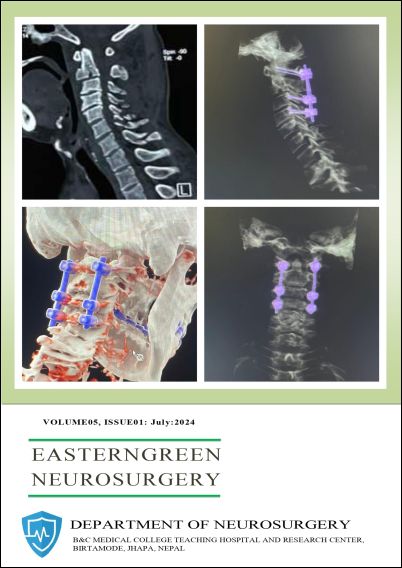
Introduction: Osteoporotic vertebral fracture is a fragility fracture due to osteoporosis and is a growing public health problem. It mainly affects postmenopausal women and men > 50 years. It significantly affects morbidity, financial condition, quality of life and mortality of patients. It presents mainly with back pain, which is mostly manageable with conservative measures. Those with unrelieved pain, severe spinal deformity or neurological impairment would require intervention. The quality of bone and surgical fitness along with associated co-morbidities of these elderly people, require special consideration, indications and appropriate modification of technique and instruments for surgical intervention. Materials and methodology: This prospective study summarizes the management of osteoporotic vertebral fractures from September 2015 to September 2021 in Nepal Medical College, Kathmandu, Nepal. The study included patients with back pain of more than 50 years old age. The backpain was evaluated clinically using visual analogue scale and Oswestry Disability Index, neurological deficits using Frankel grading system and deformity using X-ray. Other investigations included MRI, Dexa scan, Serum calcium and Vitamin D3. Risk factors for developing osteoporosis and OVF were also assessed. Results: Out of the 630 patients of more than 50 years age, presenting in neurosurgical OPD with backache from September 2015 to September 2020, 158 cases were later diagnosed to have osteoporotic spine fractures. There were 122 (77.2%) postmenopausal ladies and 36 (22.8%) gentlemen. All had backpain, with 36% having VAS score of < 3 and 64% had ODI of mild to moderate disability. The neurological deficits were present in 16.4% and mostly were Frankel grade C and D. Significant kyphoscoliosis (Cobb angle more than 20 degrees) in X-ray was present in 18 (11.3%) patients. 88 (55.7%) patients had Dexa scan and T score was less than -2.5 in 88 (56%). Serum calcium was low in (41) 26% and Vitamin D3 was low in (107) 67.7% of the patients. For backpain, all were started on non-operative management. Vertebral augmentation procedure was not available in our institute. Thus, surgery was offered in 44 (28%) of the patients but only 18 (11.4%) agreed for surgery and underwent decompression with long segment fixation. Only 48 patients remained in follow up for more than 2 years and all had satisfactory control of pain with no deterioration in deformity or neurological deficit. There were no significant short or long-term complications or mortality. Conclusion: Osteoporotic vertebral fracture is a very common reason for back pain in people of more than 50 years old affecting their livelihood. The majority responded to conservative treatment. Those indicated for surgery need special consideration in preparation, technique and devices. Preventive measures can help reduce the problem load.
Downloads
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Krishna Sharma, Maya Bhattachan, Raj Kumar Bhatta, Praveen Kumar Singh

This work is licensed under a Creative Commons Attribution 4.0 International License.